
Social Prescribing Day (9th March 2023) is an annual celebration of social prescribing, recognising link workers, local community groups and regional and national organisations which support people’s health and wellbeing.
What is social prescribing?
The Scottish Government defines social prescribing, also sometimes known as a community-based referral, as a means of enabling health professionals to refer to “resources and services within local communities with the aim of improving mental and physical health and well-being.” It is any activity in which a non- pharmaceutical intervention is recommended or provided to people with a non-clinical need such as loneliness, social isolation or low-level depression. E-health interventions are any use of digital technology to promote health, well-being, self-management or efficient and appropriate use of statutory or private health care services.
Social prescribing seeks to address our social, emotional, or practical needs holistically. Voluntary community-based organizations and digital technologies provide a range of activities that can support better health and well-being and are considered an appropriate social prescription.
Examples include:
- Volunteering
- Arts activities
- Group learning
- Gardening
- Hiking
- Befriending
- Food subscription to support food security
- Healthy eating advice
- Sports
- Sleeping Apps
- Cognitive Behaviour Apps and Platforms
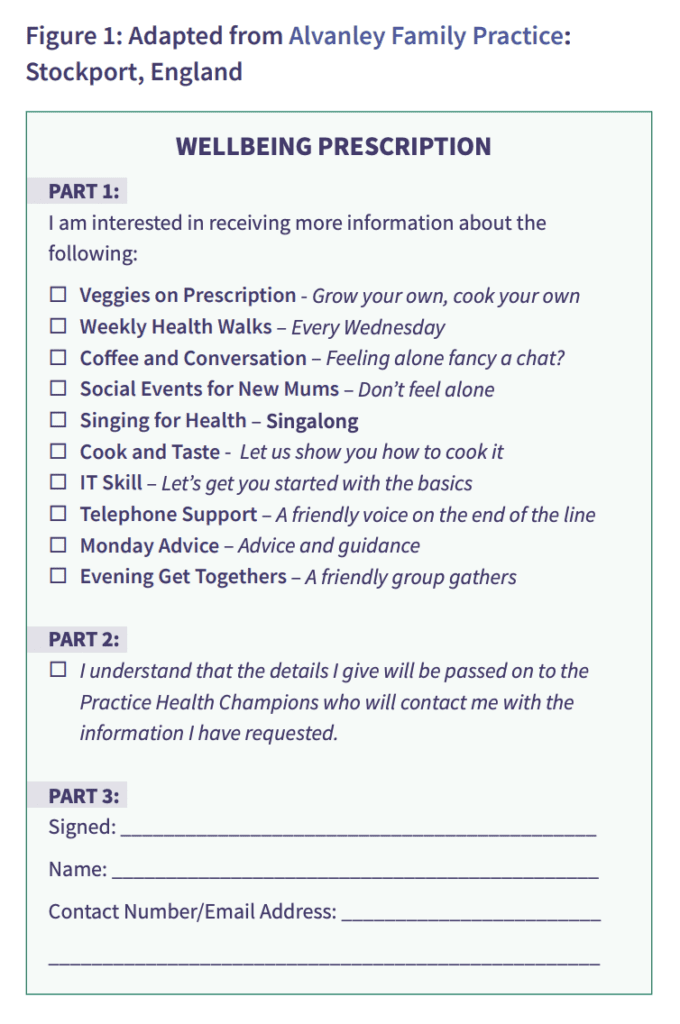
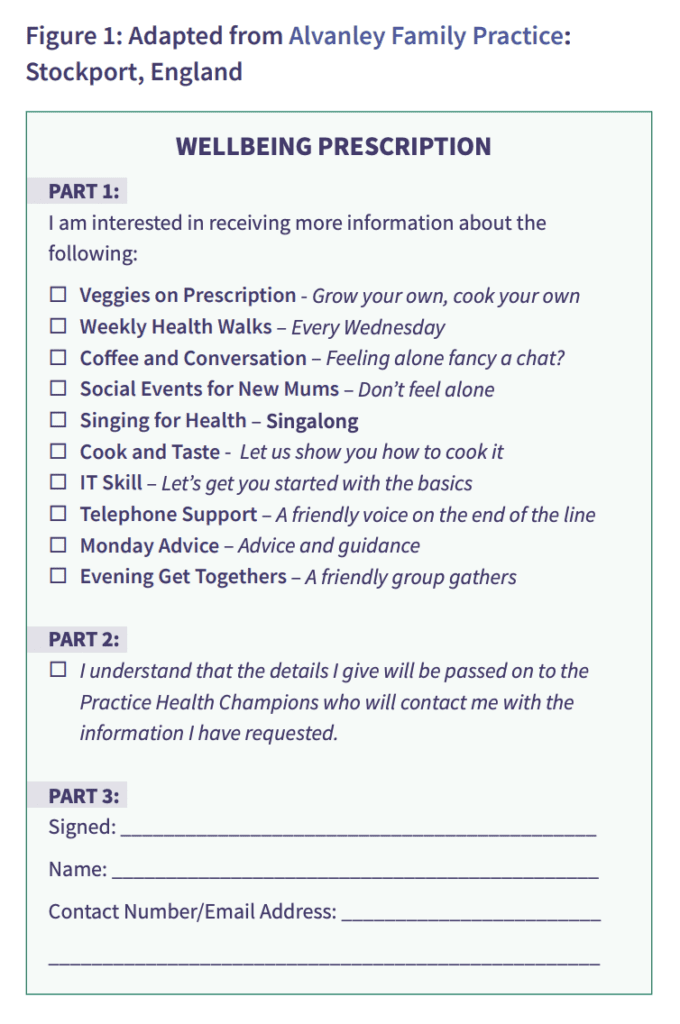
See Figure 1 for an example of a social prescription (Sourced from Ontario Hospital Association).
The Impact of Social Prescribing
Evidence has shown improvements in quality of life, emotional well-being, mental and general well-being, and levels of depression and anxiety, as well as reductions in GP appointments and admissions to acute care.
- A social prescribing project in Bristol found 6 in 10 beneficiaries reduced their GP attendance rates in the 12 months post-intervention compared to the 12 months prior to the referral.
- An evaluation of the Community Connectors Social Prescribing service in Bradford found a significant reduction in GP appointments, admissions to A&E, unplanned admissions to secondary care and a decrease in prescribing.
- The Social Prescribing Unit at the University of Westminster found a 40% reduction in visits to the GP for people who used the social prescribing service.
NHS Investments in Social Prescribing
While social prescribing schemes are not new, historically, they have been practiced on a small scale, with limited recognition from national NHS bodies. However, in recent years, there has been a renewed focus on bringing the social and medical sectors together to prioritize preventative care.
Social prescribing fits well within the ethos of Scottish health and social care policy, which calls for increased integration of services to ensure they are received when and where they are most needed (NHS Scotland, 2019). Various policy for mental health, primary care and inequalities includes impressive social prescribing targets which will increase the number of community link workers, social prescriptions and health and well-being interventions across Scotland.
The 2019 NHS Long-Term Plan identified social prescribing as a preventative initiative that would be expanded on, setting the objective that over 1,000 trained social prescribing link workers would be in place by the end of 2020/21, with the aim that over 900,000 people will be able to be referred to social prescribing schemes by 2023/24.
Connecting the Dots with a Digital Social Prescribing Solution
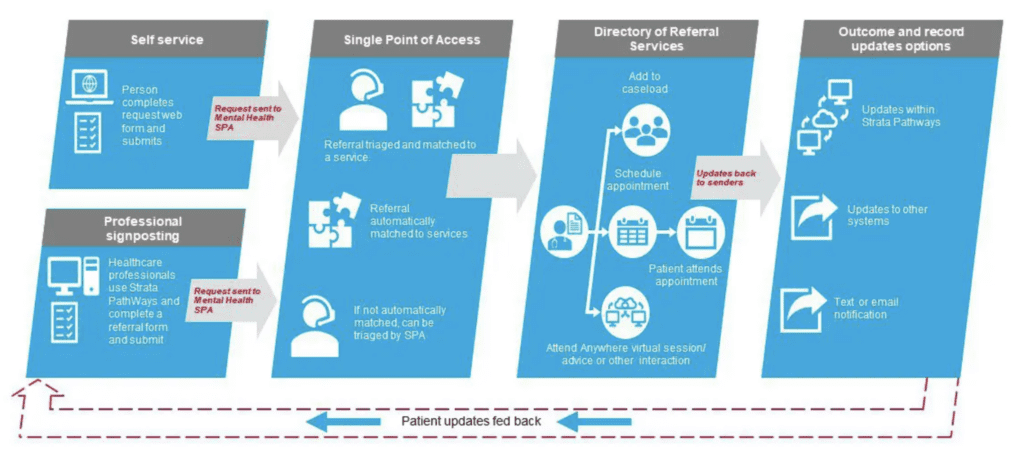
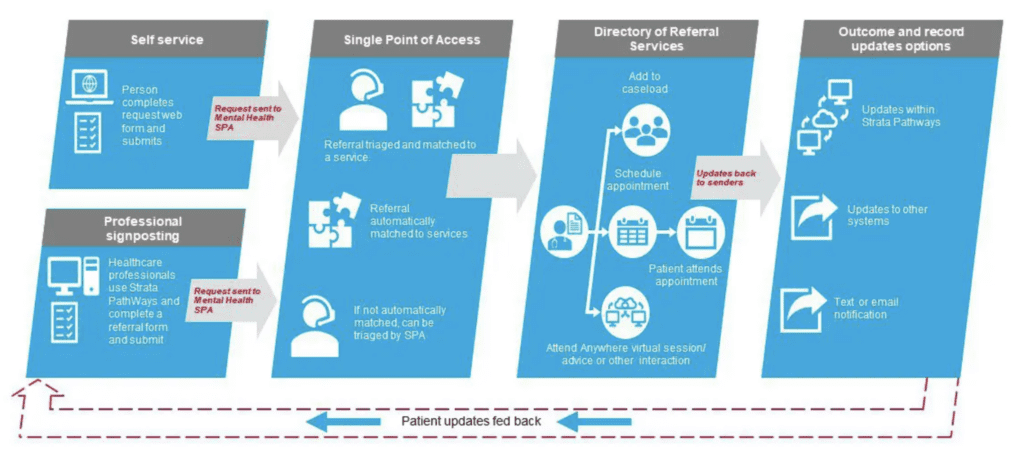
At Strata Health, we are passionate about social prescribing and working closely with our partners to design digital solutions that link the right people to the right services quickly and efficiently. As part of our efforts to support local health and care systems and their communities, we have integrated with ALISS (A Local Information System for Scotland). This web-based resource maps community assets and connects people with local sources of support that will enable them to manage their own health conditions more effectively. It is a web-based resource, which means that it is available to General Practitioners locality teams, housing, and the third sector to access information about local community support services.
With Strata PathWays’ logic matching algorithms and digital platforms, we can help to bridge the gap between primary and community care, delivering better access to services and driving more social prescribing referrals.
We’ve developed a digital single point of access (SPOA) that can be used by individuals, the Third Sector Interface (TSI), and primary/community and acute care providers to submit social prescribing referrals electronically. Once a referral has been sent, the solution will automatically triage and match the individual to the community services that best fit their needs, considering referral appropriateness and wait times. The entire referral process can be managed within the system, with updates being sent automatically to both the sender and patient every step of the way.
Implementing a social prescribing single point of access is the most effective way to:
- Improve health & well-being outcomes
- Reduce loneliness and isolation
- Reduce inequalities in health and access to resources
- Improve long term condition self-manangement
- Direct and connect individuals to the right local services
- Support integration
- Overcome information and communication silos
- Increase access to social prescribing services
- Increase referrals to community-based services
- Provide business intelligence to inform local planning and commissioning