Achieving Interoperability Between Existing eReferral Tools to Support an Integrated Health Care System in Ontario.
Overview
In 2019, Ontario’s government introduced the Ontario Health Team delivery model as part of a plan to deliver better, faster, more coordinated and patient-centred care across the province.
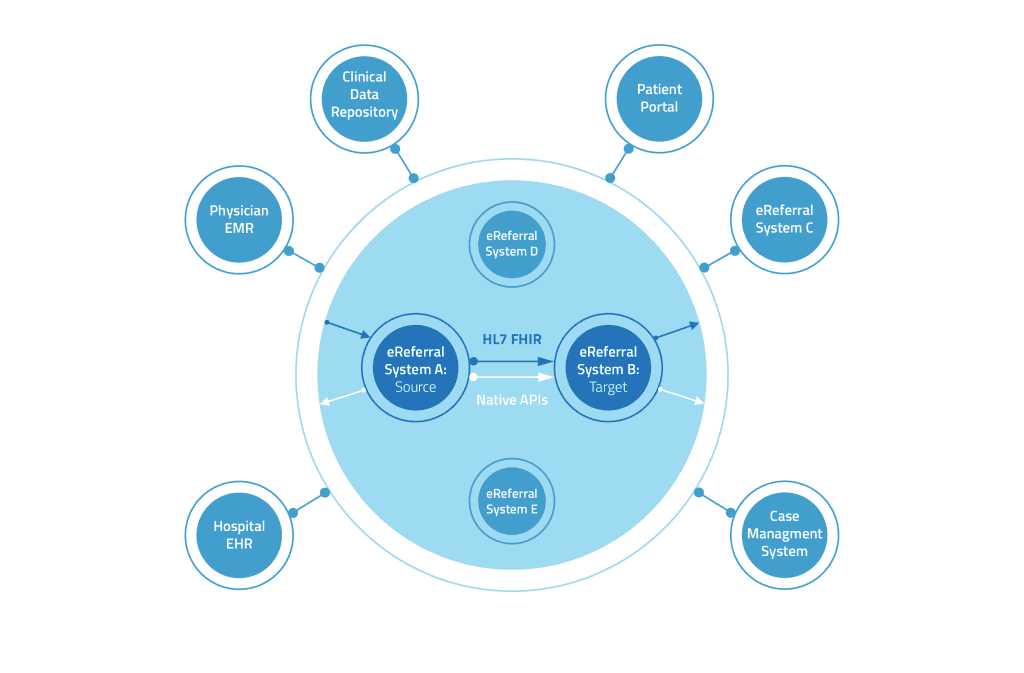
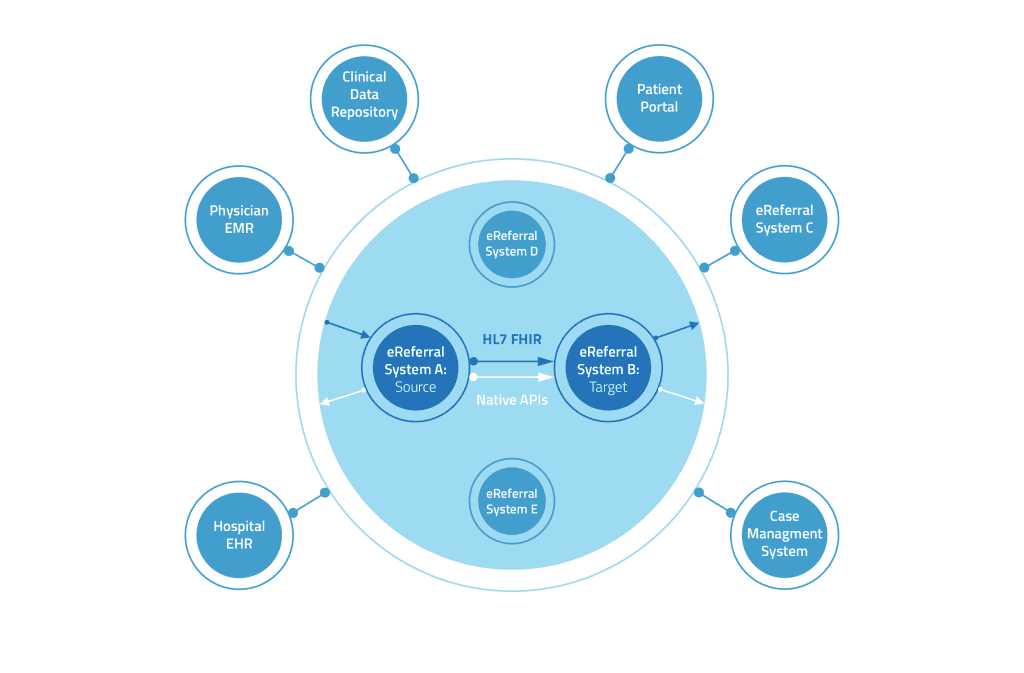
This proof of concept presents a future where patients and providers can benefit from an integrated eReferral ecosystem that connects healthcare silos, advances health system integration, transforms care delivery and ensures smoother handoffs between care settings— using existing technologies, tools and vendors. We intend to show the art of what’s possible so that all health regions in Ontario and beyond can see how their existing investments in eReferral tools can be joined with other initiatives—without requiring convergence on a single tool.
Why Do We Need eReferral Integrations?
“It is crucial that any technologies or services that are deployed in OHTs have the ability to work with the larger digital health ecosystem in Ontario so that OHTs do not run the risk of becoming “digital silos” where systems can’t talk to those of other OHTs and patient information becomes trapped.”
—Ontario Health Teams: Digital Health Playbook
Leveraging Existing Investments, Tools & Infrastructure
Best of breed solutions support varied workflows and requirements. The last 20 years have brought significant innovation in software, with many options available to the different stakeholder groups involved in the continuum of care that cater to their specific needs. We believe that this is a fundamental strength of the market and should be accommodated, rather than imposing a one-solution-for- all approach.
Seamless Experience For Patients & Clinicians Across Boundaries—
Organizational, Geographic, Political, Technological
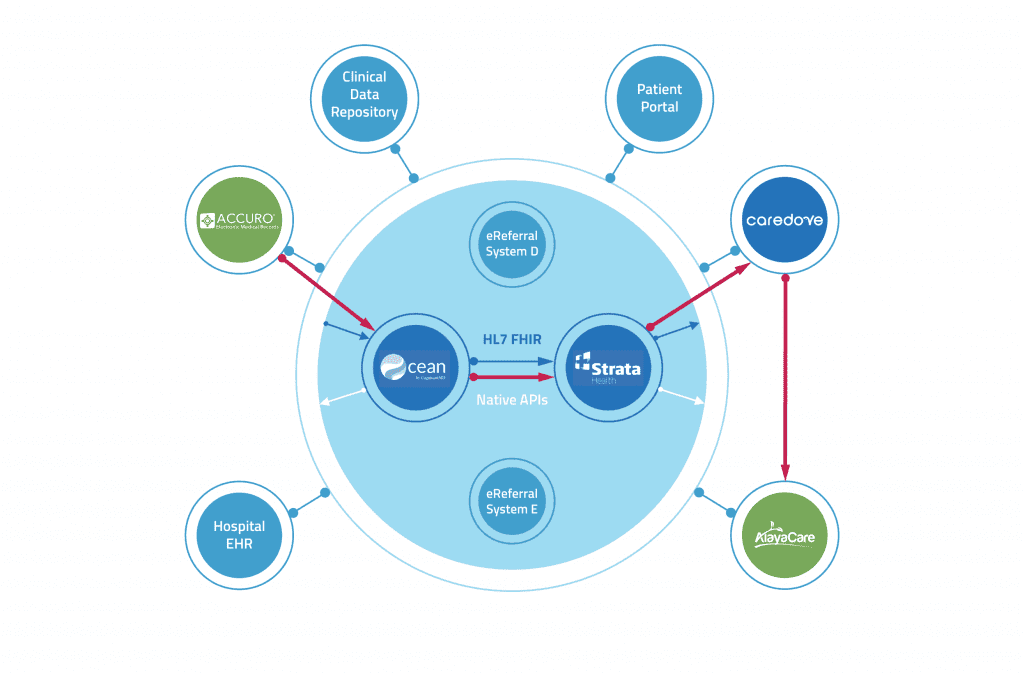
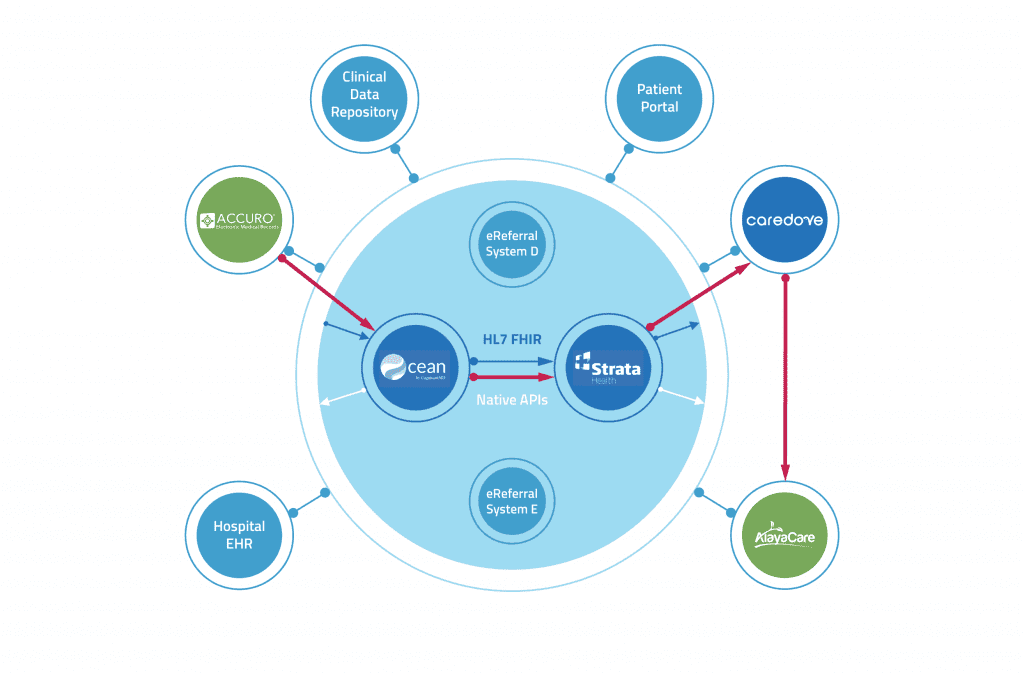
To demonstrate the power and potential of stitching together the referral ecosystem, we came together as a group of three eReferral vendors—CognisantMD, Strata Health, and Caredove—to build a proof of concept integration. Each of our respective tools have different strengths, and we represent just some of the options available in the market. We built the interface leveraging the eReferral FHIR specification, as well as our systems’ APIs. These modern tools allow for flexibility and scalability in real-time interfacing.
Our proof-of-concept aligns to the Quadruple Aim, by:
- Improving patient experience through coordinated care
- Improving provider experience through seamless interoperability and wherever possible remaining in their core clinical system
- Reducing cost through system efficiency gains (e.g., ALC) and leveraging existing investments
- Advancing population health through equitable access and reduced risk
in transitions of care
The Proof of Concept: An Integrated eReferral Ecosystem Model
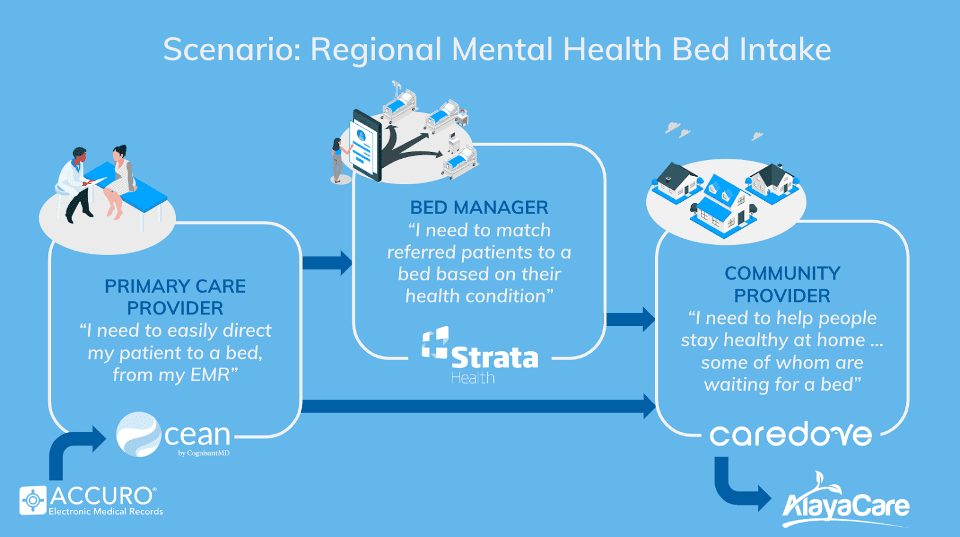
To demonstrate the art of what’s possible in Ontario and beyond, we integrated three prominent eReferral tools—Ocean eReferrals, Strata Resource Matching & Referral (RM&R), and Caredove—to show how a primary care to community workflow could work, passing through a system navigation hub. This common scenario demonstrates one of the many ways multiple eReferral tools could be intersected within a transition flow and showcases the potential of interoperability across various tools.
- Ocean eReferrals by CognisantMD: Referral platform for primary and specialist care workflows. Ocean offers integration to EMRs, included in the proof-of-concept use case from Accuro.
- Strata RM&R by Strata Health: Referral platform for bed and resource matching workflows. Strata RM&R offers integration to hospital information systems (HISs) and many other types of system.
- Caredove by Caredove: Referral management for Home and Community Care intake workflows. Caredove integrates through to AlayaCare, a prominent case management system for Home & Community Care.
The Use Case: Regional Mental Health Bed Intake
The use case for this proof-of-concept is a primary care referral for a patient needing inpatient mental health placement, where a regional intake responsible for the waitlist also coordinates supportive packages of care in the interim.
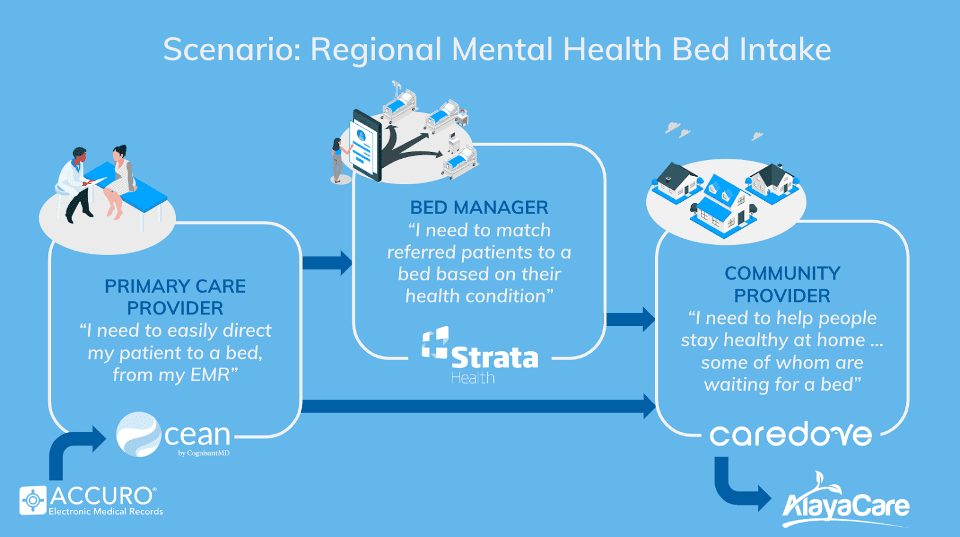
This scenario shows:
- The complexity of some transitions of care
- How implementations can keep it straightforward for some stakeholders (e.g. primary care) by keeping their workflow within their EMR while still handling the more involved aspects of others’ role in the process
(e.g. the regional intake) - How each stakeholder can have their specific workflow and system catered to in a specific use case
- How key information, like appointment status, can be conveyed back through the chain to keep everyone informed
This proof-of-concept is just a glimpse into what is possible as we collectively tackle the work of connecting all of the healthcare silos that have arose over the last few decades of rapid digital transformation. A more connected and integrated health care system is possible and we are here to help.